·
Summary: Researchers have identified a link between traumatic brain injury and intestinal changes. A new study reports the intestinal changes may contribute to increased risk of developing infections and could worsen brain damage in TBI patients.
Source: University of Maryland School of Medicine.
University of Maryland School of Medicine (UMSOM) researchers have found a two-way link between traumatic brain injury (TBI) and intestinal changes. These interactions may contribute to increased infections in these patients, and may also worsen chronic brain damage.
This is the first study to find that TBI in mice can trigger delayed, long-term changes in the colon and that subsequent bacterial infections in the gastrointestinal system can increase posttraumatic brain inflammation and associated tissue loss. The findings were published recently in the journal Brain, Behavior, and Immunity.
“These results indicate strong two-way interactions between the brain and the gut that may help explain the increased incidence of systemic infections after brain trauma and allow new treatment approaches,” said the lead researcher, Alan Faden, MD, the David S. Brown Professor in Trauma in the Departments of Anesthesiology, Anatomy & Neurobiology, Psychiatry, Neurology, and Neurosurgery at UMSOM, and director of the UMSOM Shock, Trauma and Anesthesiology Research Center.
Researchers have known for years that TBI has significant effects on the gastrointestinal tract, but until now, scientists have not recognized that brain trauma can make the colon more permeable, potentially allowing allow harmful microbes to migrate from the intestine to other areas of the body, causing infection.. People are 12 times more likely to die from blood poisoning after TBI, which is often caused by bacteria, and 2.5 times more likely to die of a digestive system problem, compared with those without such injury.
In this study, the researchers examined mice that received an experimental TBI. They found that the intestinal wall of the colon became more permeable after trauma, changes that were sustained over the following month.
It is not clear how TBI causes these gut changes. A key factor in the process may be enteric glial cells (EGCs), a class of cells that exist in the gut. These cells are similar to brain astroglial cells, and both types of glial cells are activated after TBI. After TBI, such activation is associated with brain inflammation that contributes to delayed tissue damage in the brain. Researchers don’t know whether activation of ECGs after TBI contributes to intestinal injury or is instead an attempt to compensate for the injury.
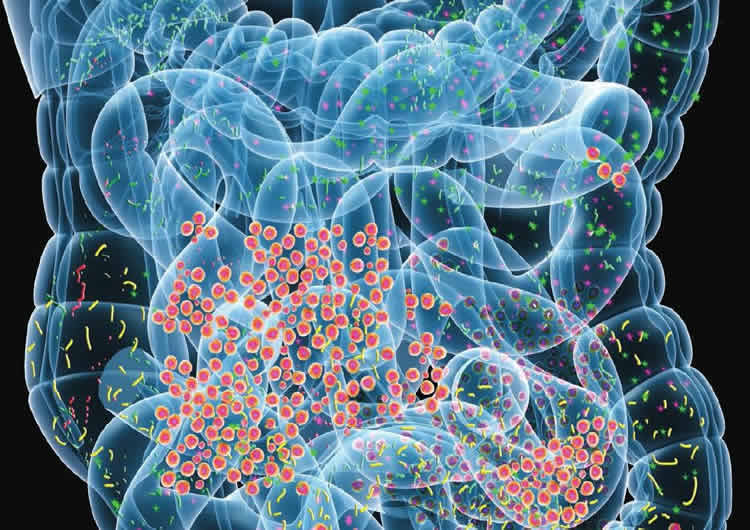
The researchers also focused on the two-way nature of the process: how gut dysfunction may worsen brain inflammation and tissue loss after TBI. They infected the mice with Citrobacter rodentium, a species of bacteria that is the rodent equivalent of E. coli, which infects humans. In mice with a TBI who were infected with this the bacteria, brain inflammation worsened. Furthermore, in the hippocampus, a key region for memory, the mice who had TBI and were then infected lost more neurons than animals without infection.
This suggests that TBI may trigger a vicious cycle, in which brain injury causes gut dysfunction, which then has the potential to worsen the original brain injury. “These results really underscore the importance of bi-directional gut-brain communication on the long-term effects of TBI,” said Dr. Faden.
Other authors of this paper include Elise Ma, a doctoral student; Terez Shea-Donahue PhD, professor of radiation oncology; Bogdan A. Stoica, MD, associate professor of anesthesiology ; and David Loane, PhD, associate professor of anesthesiology- all at UMSOM.
Source: David Kohn – University of Maryland School of Medicine
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “Bidirectional brain-gut interactions and chronic pathological changes after traumatic brain injury in mice” by Elise L. Ma, Allen D. Smith, Neemesh Desai, Lumei Cheung, Marie Hanscom, Bogdan A. Stoica, David J.,Loane, Terez Shea-Donohue, and Alan I.Fadena in Brain, Behavior and Immunity. Published online November 2017 doi:/10.1016/j.bbi.2017.06.018
[cbtabs][cbtab title=”MLA”]University of Maryland School of Medicine “Traumatic Brain Injury Causes Intestinal Damage.” NeuroscienceNews. NeuroscienceNews, 8 December 2017.
<https://neurosciencenews.com/tbi-intestines-8137/>.[/cbtab][cbtab title=”APA”]University of Maryland School of Medicine (2017, December 8). Traumatic Brain Injury Causes Intestinal Damage. NeuroscienceNews. Retrieved December 8, 2017 from https://neurosciencenews.com/tbi-intestines-8137/[/cbtab][cbtab title=”Chicago”]University of Maryland School of Medicine “Traumatic Brain Injury Causes Intestinal Damage.” https://neurosciencenews.com/tbi-intestines-8137/ (accessed December 8, 2017).[/cbtab][/cbtabs]
Abstract
Bidirectional brain-gut interactions and chronic pathological changes after traumatic brain injury in mice
Objectives
Traumatic brain injury (TBI) has complex effects on the gastrointestinal tract that are associated with TBI-related morbidity and mortality. We examined changes in mucosal barrier properties and enteric glial cell response in the gut after experimental TBI in mice, as well as effects of the enteric pathogen Citrobacter rodentium (Cr) on both gut and brain after injury.
Methods
Moderate-level TBI was induced in C57BL/6 mice by controlled cortical impact (CCI). Mucosal barrier function was assessed by transepithelial resistance, fluorescent-labelled dextran flux, and quantification of tight junction proteins. Enteric glial cell number and activation were measured by Sox10 expression and GFAP reactivity, respectively. Separate groups of mice were challenged with Cr infection during the chronic phase of TBI, and host immune response, barrier integrity, enteric glial cell reactivity, and progression of brain injury and inflammation were assessed.
Results
Chronic CCI induced changes in colon morphology, including increased mucosal depth and smooth muscle thickening. At day 28 post-CCI, increased paracellular permeability and decreased claudin-1 mRNA and protein expression were observed in the absence of inflammation in the colon. Colonic glial cell GFAP and Sox10 expression were significantly increased 28 days after brain injury. Clearance of Cr and upregulation of Th1/Th17 cytokines in the colon were unaffected by CCI; however, colonic paracellular flux and enteric glial cell GFAP expression were significantly increased. Importantly, Cr infection in chronically-injured mice worsened the brain lesion injury and increased astrocyte- and microglial-mediated inflammation.
Conclusion
These experimental studies demonstrate chronic and bidirectional brain-gut interactions after TBI, which may negatively impact late outcomes after brain injury.
“Bidirectional brain-gut interactions and chronic pathological changes after traumatic brain injury in mice” by Elise L. Ma, Allen D. Smith, Neemesh Desai, Lumei Cheung, Marie Hanscom, Bogdan A. Stoica, David J.,Loane, Terez Shea-Donohue, and Alan I.Fadena in Brain, Behavior and Immunity. Published online November 2017 doi:/10.1016/j.bbi.2017.06.018











