In case you haven’t heard, America is experiencing a severe mental health crisis. Yet, across the gamut, Americans are being deceived, exploited, manipulated, and harmed—both physically and mentally—by those entrusted to provide protection. Thanks to the unbelievable immorality surrounding the COVID-19 pandemic, the blatant failure of U.S. taxpayer-funded systems to care for its people is now unmistakable. As Big Pharma makes billions peddling pills for every ailment, prescriptions for antidepressants have risen 21 percent since the pandemic, with teenagers and young adults suffering from mental health conditions significantly more than in past generations. Regardless, amid profitable prescriptions and the tyrannical orders to be injected with mRNA gene-damaging concoctions recklessly labeled as “vaccines,” it turns out the most promising option to long-lasting health, both mental and physical, has effectively been swept under the rug. That alternative, my friends, is exercise. With little fanfare, a new study published this month in the BMJ finds that exercise is twice as effective at treating depression than antidepressant drugs. And, importantly, without the dangerous side effects and risks.
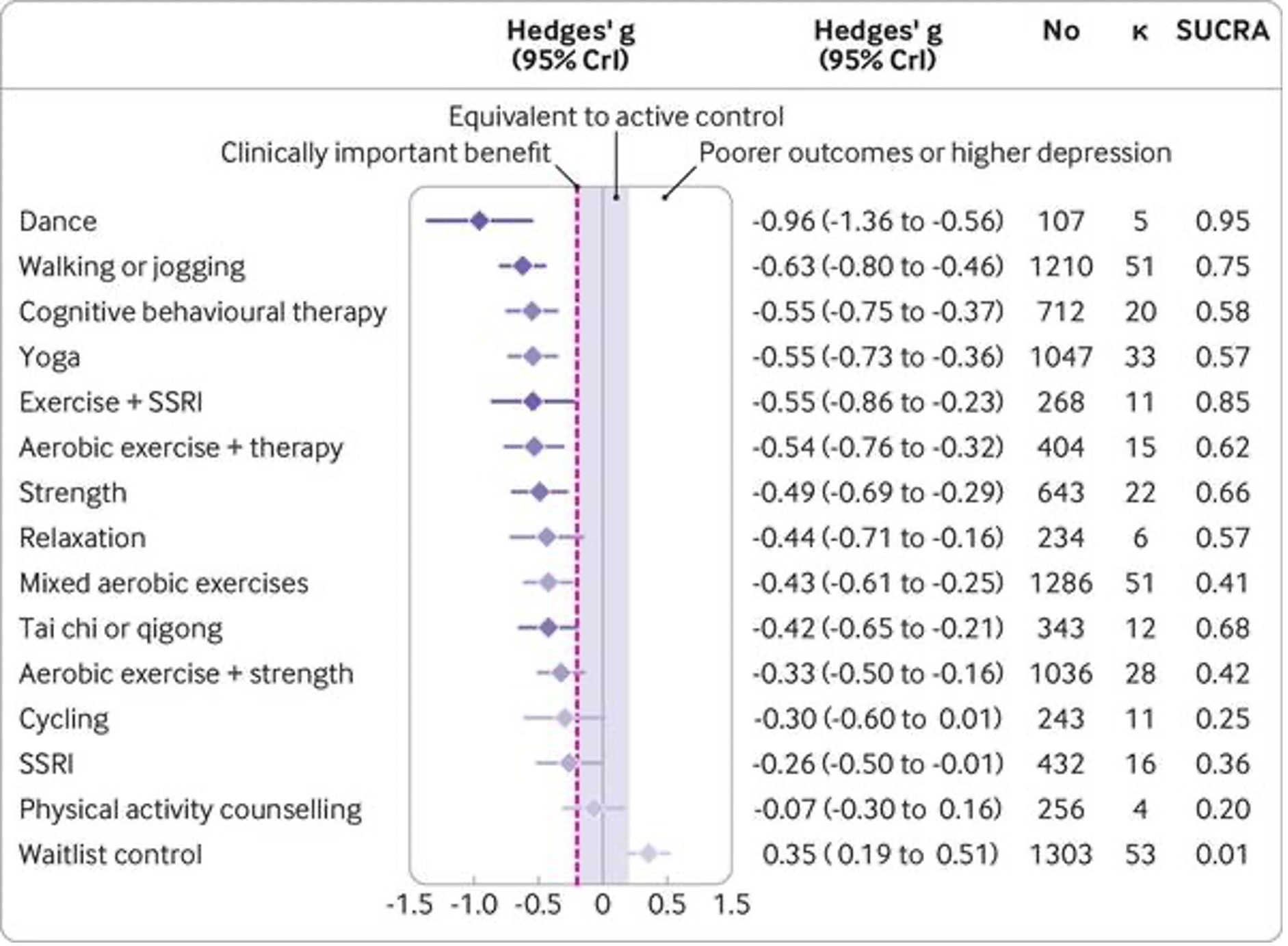
The peer-reviewed study, titled “Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials,” analyzed 14,170 people with major depression from 218 separate randomized controlled trials. Study researchers then ranked various forms of exercise by how effective they were at treating depression compared with Big Pharma’s money-making drugs. Guess what? Exercise appeared equally effective for people with and without comorbidities and with different baseline levels of depression. The study noted that “exercise may be an effective complement or alternative to drugs and psychotherapy.” Alternative! Yep, there’s no telling how many people may not need antidepressant drugs whatsoever if, from the get-go, their lives were cultivated to include healthy, all-natural, local, non-GMO foods and regular exercise.
Making it easy for anyone to participate, study researchers found that dance—with its intrinsic restorative and healing powers—is the most effective form of exercise, resulting in significant reductions in depression. The power of dance to heal depression is not surprising, considering that dance, like illness and pain, involves the culturally mediated body, emotion, and mind. A 2007 study published in The Journal of Alternative and Complementary Medicine noted that dance may promote wellness by strengthening the immune system through muscular action and physiological processes. It conditions an individual to “moderate, eliminate, or avoid tension, chronic fatigue, and other disabling conditions that result from the effects of stress.” That sounds fantastic. After all, alternative health practitioners have known for years that using dance as therapy for depression gets right to the heart of the matter, supporting the cognitive, emotional, social, physical, and spiritual attributes of an individual, allowing them to express themselves in a cathartic way.
With eyes wide open, there is no doubt that Big Pharma, the FDA, and the CDC are failing miserably at taking care of the mental health of our nation. The study pointed out that major depressive disorder is a leading cause of disability not just in the United States but worldwide. Depression lowers life satisfaction more than debt, divorce, and diabetes. Depression also exacerbates comorbidities, including heart disease, anxiety, and cancer, not to mention the comorbidities that arise from medications prescribed to treat depression.
While depression and these increased comorbidities are money in the bank for Big Pharma and create lifelong customers, they are destroying the lives of trusting Americans. Exposing the corruption, The Highwire reported last year that the Pfizer-funded “quick and dirty” checklist tool used for decades to diagnose mental illness is riddled with fraud and was devised to significantly increase Pfizer’s base of probable Zoloft prescribers. Though finally beginning to fray, the entire serotonin-depression myth led to billions in Big Pharma proceeds with no proof to back up if there was indeed a link between depression and serotonin levels. Reporting on the controversy surrounding SSRIs (a mind-boggling half a million children and adolescents in the U.S. are prescribed SSRIs each year), The Highwire’s Jefferey Jaxen wrote:
“One lesson here is when it comes to public health or mental health interventions, the public, to their detriment, will be the last to know of any true harms related to them.”
Jaxen is right about the harms surrounding SSRIs, and the list of mental health letdowns is growing. Further exposing the destructive nature in which Americans are being cared for, another recent study, also in the BMJ, revealed that the “bible” of psychiatry, the American Psychiatric Association’s esteemed Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (SSM-5-TR) is influenced by a whopping $14.2 million in undisclosed financial conflicts. In other words, the gold standard manual for treating mental health in the United States is controlled by compensation from the pharmaceutical industry. Nothing to see here, folks; move on.
As the corruption behind the handling of America’s healthcare continues to be exposed, the depression-industrial complex is sure to be unhappy with the current spotlight on the potential to remedy mental health issues with exercise. Many exercises mentioned in the study—dancing, walking, jogging, and even yoga—are free to achieve anywhere and can be tailored to the individual. While many agencies may undoubtedly state they promote exercise, the proof is in the pudding. A quick look at the propaganda blasted upon Americans from Big Pharma’s goons and U.S. government health agencies by no means promotes the straightforward and vital message “make sure you eat healthy and exercise daily.” No indeed. Here’s hoping this in-depth study boosting exercise gets the attention it deserves and exercise prescriptions immediately outpace Big Pharma’s billion-dollar drugs. With that idea in mind, the researchers concluded:
“Globally, there has been an attempt to reduce [the] stigma associated with seeking treatment for depression. Exercise may support this effort by providing patients with treatment options that carry less stigma. In low-resource or funding-constrained settings, group exercise interventions may provide relatively low-cost alternatives for patients with depression and for health systems. When possible, ideal treatment may involve individualized care with a multidisciplinary team, where exercise professionals could take responsibility for ensuring the [exercise] prescription is safe, personalized, challenging, and supported. In addition, those delivering psychotherapy may want to direct some time towards tackling cognitive and behavioral barriers to exercise. Exercise professionals might need to be trained in the management of depression (eg, managing risk) and to be mindful of the scope of their practice while providing support to deal with this major cause of disability.
Some interventions with few costs, side effects, or pragmatic barriers, such as walking and jogging, are effective across people with different personal characteristics, severity of depression, and comorbidities. Those who are able may want to choose more intense exercise in a structured environment to further decrease depression symptoms. Health systems may want to provide these treatments as alternatives or adjuvants to other established interventions (cognitive behavior therapy, SSRIs) while also attenuating risks to physical health associated with depression. Therefore, effective exercise modalities could be considered alongside those interventions as core treatments for depression.”
**WARNING: Coming off your medication can cause antidepressant withdrawal – and could set you up for a relapse of depression. Harvard Health writes about the dangers and symptoms of antidepressant withdrawal HERE.
health.harvard.edu writes, “In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks. “











